What if we could eliminate the need for lymphodepleting chemotherapy before CAR T-cell therapy?
New research, published in Molecular Therapy, introduces a unique approach to preparing CAR T-cells prior to CAR T therapy, which may eliminate the need for lymphodepleting chemotherapy.
Chimeric antigen receptor (CAR) T-cells have been commandeered for the treatment of blood cancers, including lymphomas, some forms of leukemia and multiple myeloma, and tend to be used in cases where a blood cancer has returned after treatment or a patient hasn’t responded to chemotherapy. For CAR T-cell therapy to be administered, a sample of a patient’s T-cells is collected and engineered to add CAR receptors, which are designed to target specific proteins on the surface of cancer cells. The engineered CAR cells are then reinfused and in some cases spark incredible recoveries.
However, lymphodepleting chemotherapy – the process of killing off existing T-cells to create a ‘blank slate’ for CAR T-cells – is commonly performed prior to CAR T-cell reinfusion and causes prolonged and significant side effects for patients. Headed by Assistant Professor Richard O’Neil, a research team from MUSC Hollings Cancer Center (SC, USA) – which included Graduate Student Megan Tennant – demonstrated that with the right preparatory steps, lymphodepleting chemotherapy could become a redundant step in CAR T-cell therapy.
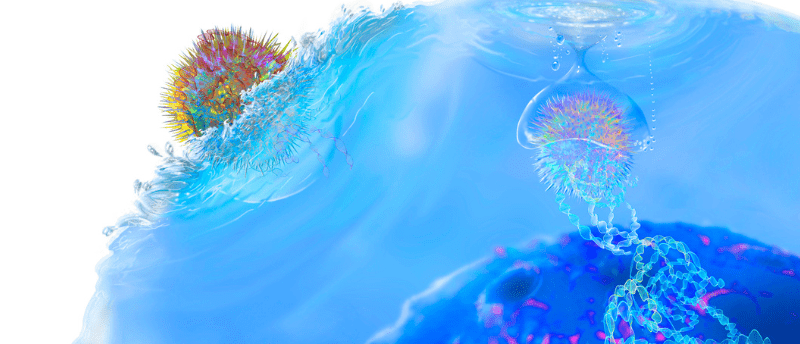
By encoding the CAR-T cells with instructions to create a hyperactive form of STAT5 protein, the CAR T-cells were prompted to engraft and begin multiplying, hence removing the need for lymphodepletion. O’Neil commented:
“We present a lot of evidence in the paper to support the notion that it’s a completely cell-autonomous process and that it’s fundamentally driven by activation of STAT5. By transiently activating STAT5 during that phase of adoptive transfer, the initial engraftment phase, you’re tricking the cells into essentially thinking they’re going into a lymphodepleted environment and so they engraft and become very functional, and they do everything they’re supposed to do. Once we saw that they’d engraft, we just benchmarked how they functioned with as many different benchmarking assays as we could, comparing it to conventional adoptive transfer using lymphodepletion as our benchmark.”
O’Neil explained that they landed on STAT5 due to its role in the cytokine signaling pathway; it’s been long understood that the interleukin cytokines IL2, IL7 and IL15 are instrumental to the engraftment process.
“We reasoned that we could recapitulate that entire signaling process at the node of STAT5, rather than trying to tickle it up at IL 15, or IL2 receptors. And by doing that, we also have more of a cell-autonomous effect where we don’t have to expose the patient to a bunch of IL7, IL15 and IL2, which can be dangerous.”
In preclinical models, the team found that their method reduced cytokine release syndrome, which is one of the most serious side effects of CAR T-cell therapy. The modified CAR T-cells carrying STAT5 also managed to control the cancer and appeared to create memory cells trained for that particular type of cancer. O’Neil explained that eliminating the need for lymphodepleting chemotherapy opens up CAR T-cell therapy for other applications and could even impact dosing schedules.
“You might be able to treat some of these more serious lupus cases. Doctors would never want to lymphodeplete somebody with lupus with the combined chemotherapies fludarabine and cyclophosphamide, but if we don’t have to lymphodeplete them anymore, then you can imagine trying out this therapy with them. Now you can imagine re-administrating dose after dose to the patient instead of ‘one and done.’ If you don’t have to lymphodeplete them, you might be able to just give them an injection every month.”
Tennant also expressed her elation for the success of the project:
“I don’t think that either of us expected that first initial experiment to work, but when we saw how well it worked and really started to conceptualize where this could go and how important this could be, it was exciting.”
O’Neil is now working with the MUSC Lupus Erythematosus Research Group (SC, USA) to develop clinical trials and is even conversing with biotechnology companies working in the CAR-T space. He praised Tennant’s diligence in perusing the project:
“This has been Megan’s labor of love. It’s actually been pretty remarkable. She just joined my lab when I came here two years ago, so this entire project came from conception to fruition in two years, which is pretty amazing and definitely shows what a talented and hard-working scientist Megan is.”