Understanding how biologics trigger immune responses: T-cell-dependent vs T-cell-independent pathways
Author: Indiwari Gopallawa, Integrated Bioanalysis, Clinical Pharmacology and Safety Sciences, AstraZeneca (MD, USA)
Indi Gopallawa is a Senior Scientist in the Integrated Bioanalysis department at AstraZeneca (MD, USA), where she leads the development and validation of bioanalytical assays to support multiple programs in AstraZeneca’s pipeline. Before joining AstraZeneca, Indi completed her postdoctoral training at the University of Pennsylvania (PA, USA). There, she focused on developing cell-based assays to identify key inflammatory signaling mechanisms that contribute to lung diseases such as COPD, asthma and cystic fibrosis. She earned her PhD in biochemistry from Michigan State University (MI, USA).
Keywords: Immunogenicity, T-cell-dependent and independent mechanisms, Anti-drug antibodies, and AI/ML.
Immunogenicity
Immunogenicity refers to the immune system’s response to foreign substances, including therapeutic proteins [1]. Anti-drug antibodies (ADA) are produced when the immune system is activated by these proteins, which serve as a metric for assessing immunogenicity [2]. Unlike small molecule drugs, biologics are complex entities, making them prone to intricate immune reactions. These adverse responses can have significant clinical implications, including anaphylaxis, reduced efficacy and neutralization of both the therapeutic protein and its endogenous human counterpart [3]. However, in recent years, the generation of humanized monoclonal antibodies has significantly reduced immunogenicity, particularly its severe indications.
Assessing potential immunogenicity against therapeutics is integral to the drug development process to manage clinical implications. Various assay methodologies are used to detect ADA, including ELISA, radioimmunoassay, surface plasmon resonance and electrochemiluminescence (ECL)-based bridging assays. Among these, the bridging assay utilizing the Meso Scale Discovery platform is widely favored for its broad dynamic range and high sensitivity in detecting low levels of ADA [4]. In this method, the sample is mixed with biotin-labeled and ruthenium-labeled drugs. If ADA is present in the sample, it will bind to the biotin-labeled and ruthenium-labeled drug molecules, forming a ‘bridge’ between them. The mixture is then added to a plate with immobilized streptavidin. Streptavidin has a high affinity for biotin, so it captures the biotin-labeled drug within the complex. Once the complexes are captured on the surface, the plate is subjected to an ECL detection system. When an electrical current is applied, the ruthenium tag emits light. The amount of light emitted is measured and is proportional to the amount of ADA in the sample [5]. The more ADAs present, the more complexes are formed and captured, resulting in a stronger signal. During assay development and validation, a positive control is employed to ensure assay performance. A significant advantage of this method is its ability to detect all isotypes of ADA.
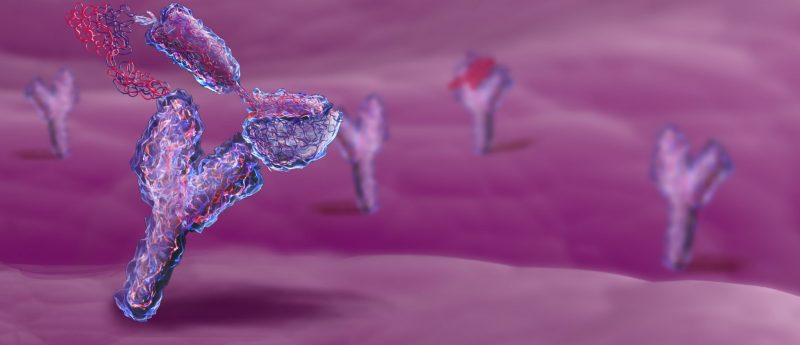
T-cell-dependent vs T-cell-independent pathways
The immune system employs two primary mechanisms to generate ADA against therapeutic proteins: T-cell-dependent and T-cell-independent pathways. T-cells play distinct roles in initiating an immune response. CD8+ T-cells are involved in cell-mediated immunity, directly attacking infected or cancerous cells. In contrast, CD4+ T-cells, also known as helper T-cells, perform functions such as secreting cytokines and activating B-cells. These activated B-cells then contribute to humoral immunity by producing antibodies. In the T-cell-dependent pathway, B-cells require CD4+ T-cell co-stimulation to initiate antibody production. Conversely, the second pathway operates independently of CD4+ T-cells, with B-cell activation occurring autonomously. Some clinical studies have shown that IgG antibodies are generated predominately via the T-cell-dependent pathway in response to most therapeutics [6].
Upon administration of a therapeutic protein, it undergoes processing, leading to the presentation of peptides on both MHC class I and MHC class II molecules by antigen-presenting cells (APCs). Naive T-cells continuously circulate within lymph nodes and encounter these peptides. When the T-cell receptor (TCR) on naive T-cells recognizes the antigen presented on MHC molecules on the surface of APCs, it initiates the activation process, leading to differentiation into effector T-cells. These effector T-cells, primarily helper T-cells (CD4+ T-cells), then undergo clonal expansion, (rapid proliferation) to induce a robust cellular response [7]. Meanwhile, naive B-cells in lymph nodes require dual signals for proliferation and differentiation into antibody-secreting plasma cells. The initial signal is initiated by the direct binding of the antigen to B-cell receptors expressed on naive B-cell surfaces. Following internalization and processing, the peptides are presented by MHC class II molecules. The second signal for B-cell activation is provided by helper T-cells, specifically by the T follicular cell subtype (there are different CD4+ helper T-cell populations). This interaction involves the binding of TCR to the peptide presented by the MHC class II complex on the surface of naive B-cells, along with the engagement of CD80/CD86 on B-cells with CD28 on T-cells (co-stimulatory receptors). The interaction between B- and T-cells induces the expression of CD40L on the surface of helper T-cells that interact with CD40 receptors on B-cells. This interaction leads to the secretion of B-cell stimulatory cytokines. These events activate B-cells, transforming them into antibody-secreting plasma cells. These responses are highly regulated, and the T-cell-dependent pathway is critical for producing an antibody that binds to an antigen with high affinity (affinity maturation) and plays a role in switching the antibody class from IgM to IgG, or other heavy chain classes including IgA, IgD and IgE [6].
T-cell-independent responses are initiated by non-protein antigens that cannot activate the T-cell-dependent pathway. These antigens are often enriched with polysaccharide and/or lipid structures, that lead to the production of low-affinity IgM antibodies. In this pathway, B-cells swiftly produce antibodies without requiring secondary signals from CD4+ T-cells [8]. Highly repetitive antigens on the surface of pathogens can activate specific B-cell populations by crosslinking B-cell antigen receptors, initiating a signaling cascade. Unlike in the T-cell-dependent pathway, this pathway lacks affinity maturation, resulting in primarily IgM-type responses.
Therapeutic proteins can trigger immune reactions that vary in intensity. Depending on the nature of the trigger, the immune response can generate transient low-affinity IgM antibody responses or high-affinity responses by class switching to IgG. The consequences of these immune reactions can vary widely, from minimal effects to severe and life-threatening outcomes.
Using AI/ML to identify T-cell epitopes
An epitope is a segment of an immunogenic protein, such as therapeutic proteins or peptides, that the immune system can recognize and initiate an immune response against. T-cell epitopes are specific peptide fragments recognized by TCRs after an antigen, like a therapeutic protein, has been processed within a cell, bound to an MHC molecule and presented on the surface of antigen-presenting cells [9]. Immune responses to T-cell epitopes can produce antibodies that may neutralize the therapeutic protein, reducing its efficacy. To mitigate such immune responses to T-cell epitopes, it is desirable to eliminate MHC-binding epitopes and increase the host sequence content within the therapeutic product without disrupting essential interactions such as proper folding and function. Computational methods such as in silico tools now enable the design of less immunogenic proteins, creating a novel class of therapeutics with increased tolerability in patients [10]. AI/ML tools can predict T-cell epitopes with relative precision, allowing protein therapeutics into higher-risk and lower-risk categories based on their T-cell epitope content before clinical development, thus improving clinical outcomes.
References:
- Bawa R, Szebeni J, Webster TJ & Audette GF. Immunogenicity assessment for therapeutic protein products 1. (1st Edition). Immune Aspects of Biopharmaceuticals and Nanomedicines: Jenny Stanford Publishing; p537–583 (2019).
- Baker MP, Reynolds HM, Lumicisi B & Bryson CJ. Immunogenicity of protein therapeutics: The key causes, consequences and challenges. Self Nonself. 1(4), 314–322 (2010).
- Mahanty S, Prigent A & Garraud O. Immunogenicity of infectious pathogens and vaccine antigens. BMC Immunol. 16(31) (2015).
- Du J, Yang Y, Zhu L et al. Method validation of a bridging immunoassay in combination with acid-dissociation and bead treatment for detection of anti-drug antibody. Heliyon. 9(3), e13999 (2023).
- Partridge MA, Purushothama S, Elango C & Lu Y. Emerging technologies and generic assays for the detection of anti-drug antibodies. Immunol. Res. 1, 6262383 (2016).
- Jawa V, Terry F, Gokemeijer J et al. T-cell dependent immunogenicity of protein therapeutics pre-clinical assessment and mitigation-updated consensus and review 2020. Immunol. 11, 1301 (2020).
- Jawa V, Cousens LP, Awwad M, Wakshull E, Kropshofer H & De Groot AS. T-cell dependent immunogenicity of protein therapeutics: Preclinical assessment and mitigation. Immunol. 149(3), 534–555 (2013).
- Allman D, Wilmore JR & Gaudette BT. The continuing story of T-cell independent antibodies. Rev. 288(1), 128–135 (2019).
- Mazor R, King EM & Pastan I. Strategies to reduce the immunogenicity of recombinant immunotoxins. J. Pathol. 188(8), 1736–1743 (2018).
- Mattei AE, Gutierrez AH, Seshadri S et al. In silico methods for immunogenicity risk assessment and human homology screening for therapeutic antibodies. mAbs. 16(1), 2333729 (2024).
Disclaimer: the opinions expressed are solely my own and do not express the views or opinions of my employer.