‘Heart-on-a-chip’ could assist in the screening of drugs

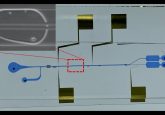
A research team form UC Berkeley (CA, USA) have developed a ‘heart-on-a-chip’ system, consisting of a network of cardiac muscle cells contained in a 1 inch-long device, which can be used to effectively model human heart tissue. It was demonstrated that the system could be used as a drug-screening tool by testing its reaction to cardiovascular drugs. Their findings where recently published in Scientific Reports.
The team, led by Kevin Healy (bioengineering professor at UC Berkeley), noted a high failure rate of the use of nonhuman animal models to predict human reactions to new drugs. This high failure rate is largely due to intrinsic differences in biology between species.
The heart cells utilized in the device were derived from human-induced pluripotent stem cells – adult stem cells that can be manipulated to form many different types of tissues. This cardiac microphysiological system, or ‘heart-on-a-chip’, was designed to have a three-dimensional structure comparable to the geometry and spacing of connective tissue fiber in a human heart. The differentiated human heart cells were added into a loading area, in which the system’s confined geometry assisted in alignment of the cells in multiple layers, in a single direction.
To mimic the exchange of nutrients and drugs in human tissue, which is facilitated by blood vessels, microfluidic channels were established on either side of the cell. This setup could eventually allow researchers to monitor the removal of metabolic waste from the cells.
Some 24 hours after the heart cells were loaded into the chamber, they began to beat at a normal physiological rate of 55—80 beats per minute. To test the systems, researchers monitored the reaction of the heart cells to four common cardiovascular drugs: isoproterenol, E-4031, verapamil and metoprolol. They discovered that responses after exposure to the drugs were predictable, with heart rate reducing/increasing in line with the administered drugs desired effect.
The team believes that their device could be altered to model human genetic diseases or to screen for an individual’s reaction to a drugs. Healy hopes that these chips could ultimately replace the use of animals to screen drugs for safety and efficacy.
Looking to the future, the team is studying whether the system could be used to model more complex multiorgan interactions. “Linking heart and liver tissue would allow us to determine whether a drug that initially works fine in the heart might later be metabolized by the liver in a way that would be toxic,” commented Healy.
Source: Bioengineers put human hearts on a chip to aid drug screening.