From brain biopsies to liquid biopsies: a next-generation platform using extracellular vesicles to detect brain disorders
Advanced analysis of extracellular vesicles from blood can identify biomarkers associated with brain disorders, offering a novel diagnostic platform.
A research team, led by David Walt from the Wyss Institute (Wyss) at Harvard University (MA, USA) and Brigham and Women’s Hospital (MA, USA), has made a significant breakthrough in the early diagnosis of brain disorders by analyzing extracellular vesicles (EVs) from blood. This advancement offers new insights into liquid biopsies for brain disorders such as Parkinson’s disease (PD) and Alzheimer’s disease. Their findings are published in the Proceedings of the National Academy of Sciences.
Brain disorders affect over one in three people globally, and begin in patients long before the first clinical symptoms become apparent. This pre-symptomatic period presents a critical window for intervention, where timely treatment could potentially slow or even halt the progression of these diseases. While several biomarkers have been linked to the early stages of brain disorders, there are currently a lack of diagnostic tools capable of accurately detecting these biomarkers during pre-symptomatic stages.
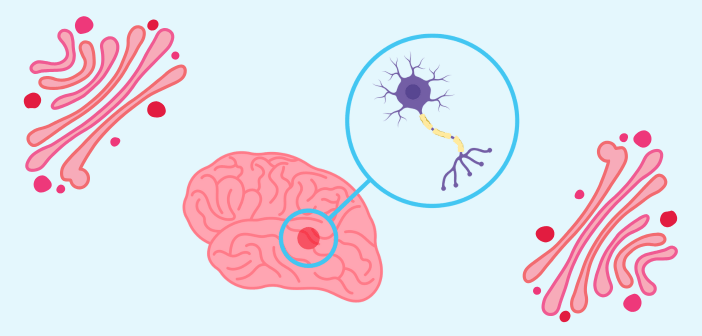
EVs are membrane-bound sacs produced by all cell types and released into extracellular fluids. The molecule composition inside EVs is cell-type specific. Because of this, EVs could carry protected biomarkers that might indicate the early onset of brain disorders.
However, the presence of EVs in blood is low and current EV isolation techniques are not effective in distinguishing EVs from free proteins. Measuring EV proteins from both total EVs and isolating brain EVs from blood therefore presents significant challenges. Consequently, determining whether a protein that is detected after EV isolation is contained within the EV is difficult.
“To answer the conceptually simple but technically challenging question of what percentage of a given protein (such as ⍺-synuclein) present in plasma is inside of EVs relative to outside, we used SEC (size exclusion chromatography) isolation methods that we previously developed to isolate most EVs from plasma together with an optimized ‘proteinase protection assay’, where we use an enzyme to gently but efficiently chew all proteins off the surface of isolated EVs, while leaving the membrane-enclosed EV interior intact,” explained Dima Ter-Ovanesyan, a Senior Scientist at Wyss and co-first author.
The team used these developed methods to achieve ultrasensitive protein measurement and assess both total and phosphorylated α-synuclein within EVs extracted from samples of patients with PD and Lewy body dementia. α-synuclein is a presynaptic neuronal protein that is linked genetically and neuropathologically to brain disorders. Interestingly, it has been observed that the ratio of phosphorylated ⍺-synuclein to total ⍺-synuclein is two to three times greater within EVs compared to outside of EVs.
“This was extremely exciting because it suggests that EVs may protect the phosphorylation state of proteins from circulating phosphatases that would otherwise erase this highly informative mark,” explained Tal Gilboa, a postdoctoral fellow at Wyss.
The team is now investigating the potential of their assays to distinguish between PD patients and healthy individuals.
“The work by David Walt’s team presents a technological tour-de-force that brings us closer and closer to a next-generation diagnostic platform with extraordinary potential. At this point, we are not far from using these extremely rich and telling cell-derived vesicles as a window to peak into the brains of patients without requiring surgery,” commented Donald Ingber, the Wyss Founding Director.