Bispecific antibodies are ‘switching’ up immunotherapy
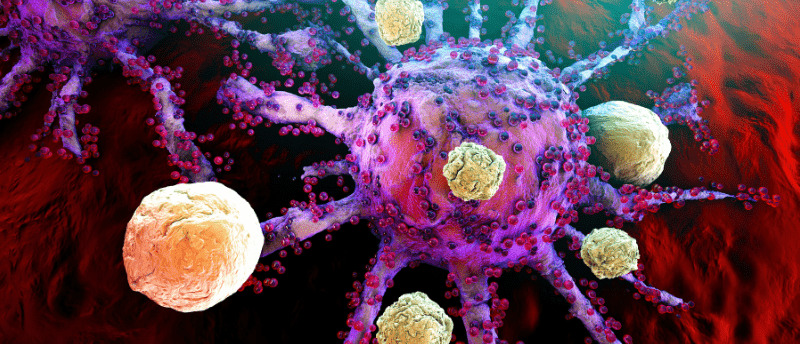
Bispecific antibodies have emerged as effective cancer immunotherapies, showing promise in treating blood-borne cancers and are being evaluated for solid tumor therapy. Bispecifics possess two binding sites that bind two different antigens, facilitating the engagement of two targets using a single molecule. Most approved bispecific antibodies bridge the gap between the ‘effector’ i.e. the T-cell and the cancerous target cell. The proximity of the two cells prompts the T-cells to attack the cancer cell. However, bispecific antibodies can suffer from cell-specific targeting limitations, known as ‘on-target off-tumor toxicity’, meaning that other healthy cells are damaged in addition to the target cell.
A research team led by Michael Mitchell, University of Pennsylvania (PA, USA), has identified a method to evade ‘on-target off-tumor toxicity’ using a bispecific T-cell nanoengager, equipped with an ‘off-switch’. The team published their work in Nature Biomedical Engineering.
“We’re excited to show that bispecific antibodies can be tweaked in a way that allows us to tap into their powerful cancer-killing potential without inducing toxicity to healthy tissues,” explained Mitchell, Associate Professor of Bioengineering at Penn State’s School of Engineering and Applied Science. “This new controllable drug-delivery mechanism, which we call switchable bispecific T cell nanoengagers, or SiTEs, adds this switchable component to the antibody via administering an FDA-approved small-molecule drug, amantadine.”
Former Postdoctoral Researcher in the Mitchell Lab and first author Ningqiang Gong, explained that the team aimed to harness the ability of bispecific antibodies to induce tumor cell toxicity but turn off the therapy to prevent the destruction of non-cancer cells. To achieve this, they considered the bispecific’s binding mechanism; one arm binds to a specific antigen on cancer cells, in this case HER2, and the other binds to the CD3 receptor on T cells.
“We then applied principles from supramolecular chemistry, namely how large proteins can be assembled into a range of structures that can then be disassembled by tiny molecules, to engineer our SiTEs such that they could be broken down once amantadine is introduced,” explained Gong.
You may also be interested in:
- Rapid Generation of Bispecific Antibodies for High-Throughput Screening with SpyLock Technology
- World Immunotherapy Congress 2024
- Technology Digest: Antibody engineering and SpyTag-SpyCatcher technology
The SiTEs can be comprised of two large molecules: PEG-phenyl, which attaches to a part of CD3, and PEG-Beta-CD, which conjugates to HER2. The bonding agent the team synthesized was novel in that when the correct concentrations of each molecule are present, the small molecule drug amantadine bonds with PEG-Beta-CD with high affinity, disengaging the T-cells from the tumor cells. This high affinity prompts the detachment of the components, both in vitro and in vivo.
“Additionally, we found that higher doses of SiTEs can induce an in situ vaccine effect,” Gong stated, “meaning the immune system is trained to generate a tumor-specific mounted defense to clear all other tumors, and, in the event of a relapse, the body has the tools to similarly tackle future tumors.”
If this detachment is possible in larger animals the team hopes to be able to move on to clinical trials. As this work was done on breast cancer tumor cells, the team also wants to try to apply this strategy to other solid tumor models to see if it can be applied to treat other cell types.
Source: Gong N, Han X, Xue L et al. Small-molecule-mediated control of the anti-tumour activity and off-tumour toxicity of a supramolecular bispecific T cell engager. Nat. Biomed. Eng. doi:10.1038/s41551-023-01147-6 (2024) (Epub ahead of print).