An overview of the challenges and implementation of ELISpots: an interview with Michelle Miller
In this interview, Michelle Miller (BioAgilytix; NC, USA) provides a basic overview of an ELISpot assay and how the method is used for the safety testing of therapeutics. She discusses some of the technical challenges with using ELISpots in regulated bioanalysis including the appropriate handling of clinical samples, quick isolation of peripheral blood mononuclear cells after sample collection and sample logistics including proper control of temperature. She also reveals her hope for more specific guidance on the use of ELISpot assays for regulated bioanalysis.
-
Can you provide a basic overview of an ELISpot assay?
Enzyme-Linked Immunosorbent Spot or ‘ELISpot’ assays measure cytokines or antibodies produced by activated immune cells using an enzymatic detection method. A variation of this is the FluoroSpot, which follows the same general methodology but has a fluorescent detection readout. For cytokine ELISpots, the plates contain a membrane that is coated with antibodies to capture the analyte of interest. Cells are stimulated with antigen peptides directly within the ELISpot plate wells and as the responding cells produce cytokines, these cytokines are captured by the antibodies on the membrane. After the method-specific incubation period, samples are removed from the wells and the membrane is developed with the enzymatic or fluorescent detection reagents. The positive cells are visualized by the concentrated foci of cytokines, visualized as spots in the wells, hence the name ELISpot.
-
How is the ELISpot method utilized for safety testing of therapeutics?
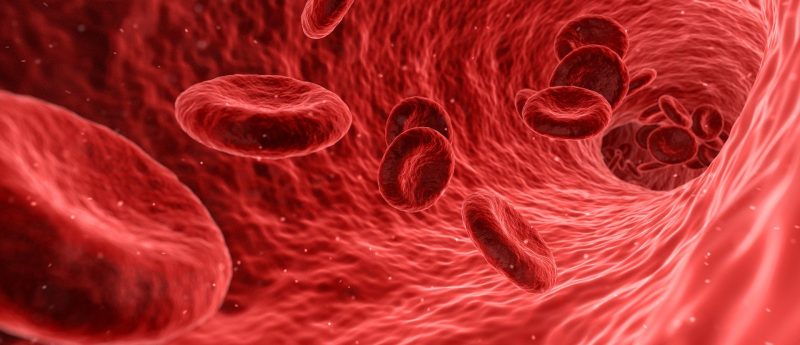
One common application for ELISpot assays is to detect T cell activation by a therapeutic. For example, when a patient receives an adeno-associated virus (AAV) gene therapy, it will enter the patient’s cells and deliver a transgene that can be translated into a protein. The proteins from both the AAV capsid and the transgene product can be processed and presented by the transduced cell, potentially inducing an immune response. To monitor this process during clinical trials, patient samples are collected and peripheral blood mononuclear cells (PBMCs) are isolated from the blood. The PBMCs are then incubated with peptides generated from the therapeutic proteins, mimicking the processing and presentation of these proteins in vivo. The immune cells that specifically recognize these peptide sequences will be reactivated and begin producing cytokines, which are captured on the ELISpot plates, allowing each activated cell to be visualized as a spot at the end of the assay. The number of cytokine-producing cells can be reported as the number of positive cells or ‘spots’ per number of cells plated in the assay.
-
What are some of the technical challenges with using ELISpots in regulated bioanalysis?
There are several unique considerations for designing an ELISpot assay in support of regulated bioanalysis, the first being the appropriate handling of clinical samples. The PBMCs required for testing must be isolated from the patient’s blood as quickly as possible following sample collection. Most clinical sites are not equipped to perform isolation so samples must be shipped to a central laboratory or other vendor. Although performing the isolation of cells in a single laboratory improves consistency across the study, the conditions during shipment and the speed of delivery are critical for maintaining the integrity of the samples. Once isolated, the PBMCs are cryopreserved and stored in liquid nitrogen until use. The leading issues our clients experience are problems with sample logistics including the proper control of temperature and time of transit.
Another challenge of ELISpot testing is the volume of sample required from the subject for each timepoint. PBMC count in a healthy adult varies but is typically in the range of 1.5e6 to 3e6 cells per mL of blood. When considering the concentrations of cells needed per well for an ELISpot assay, the number of replicate wells, the positive and negative controls and the preference for having more than one sample aliquot in case of repeat analysis, a typical sample volume from a patient would ideally be more than 10mL of blood. This can be a challenge, particularly in pediatric studies where collection volumes are limited or in cases where patients have undergone therapy to stimulate the immune system prior to therapy.
-
What type of data do you get from an ELISpot assay?
This ELISpot assay is quantitative, providing the number of antigen-specific cells within a defined cell population. For a simple cytokine ELISA with PBMCs, selecting an inflammatory cytokine such as IFNγ or TNFα can inform you of the basic type of immune response occurring. Sorting or purifying populations of cells on the front end of the assay so that you are plating only CD4+ T cells for example, can provide an additional layer of specificity for the data output. For a dual-plexed assay, the number of dual or single cytokine-producing spots can be identified. FluoroSpot assays allow for multiplexing more than two analytes, which produces data sets with additional complexity. Comparing data from patient samples collected pre-dose and post-dose provides a measure of the change in cell-mediated immunogenicity due to treatment with the therapeutic. This can be used in conjunction with assays measuring humoral immunogenicity at matching sampling times to form a full picture of the patient-specific immune response profile.
-
Do you foresee any changes to the implementation of ELISpots in the future?
The number one thing that I would like to see in the near future is more specific guidance on the use of ELISpot assays for regulated bioanalysis. I think we have done a great job as an industry of coming together and discussing the challenges and technical strategies around these assays, but we still lack clear guidance from regulatory authorities. I would like to see more details around the expected technical approaches as well as the clinical strategies for ELISpot use. It would be great to clarify some of the aspects of measuring cellular immunogenicity and make sure that drug development teams are able to get the most useful data from these testing programs to streamline delivery of important therapeutics to the people who really need them.
About the speaker

Michelle Miller, PhD, DABT
Scientific Officer, Director
BioAgilytix (NC, USA)
Dr. Miller has over a decade of experience working in the fields of immunology and toxicology. With a strong background in project management, Dr Miller previously served as an Associate Director of Bioanalytical Operations at BioAgilytix.
Prior to BioAgilytix, Michelle worked as a study director leading GLP toxicology and immunotoxicology studies as a lead investigator in the toxicology field developing high throughput screening assays, and as an R&D scientist in the pharmaceutical industry.
In association with: